Abstract
BACKGROUND: Robust immune reconstitution following allogeneic hematopoietic cell transplantation (HCT) has been associated with better outcomes in meeting the challenges of infections and malignancy relapse. One major component of reconstitution is the depth of diversity of the T cell receptor (TCR) repertoire but it is not clear what time frame is relevant and how much diversity is critical.
HYPOTHESIS: We hypothesized that at 90 days and/or 180 days, repertoires with more restricted diversity would predict for the increased risk of relapse and infections in the first year post-transplant. We herein present the results related to the risk of relapse.
METHODS: Patients with multiple myeloma were conditioned with reduced intensity conditioning (77%) and non-myeloablative (23%) with FM (13.6%), FluCyTBI (18.2%), FluMelVel (63.6%) and FluCy (4.6%). At day 0, they received a matched related (72.7%) or unrelated donor (27.3%) peripheral blood (86-89%) or bone marrow (11-14%) stem cell transplant. Peripheral blood samples were collected from the patients at day 90 and 180 (+/- 30 days) post-transplantation. Peripheral blood mononuclear cells isolated on ficoll-hypaque gradients were cryopreserved and sent to Adaptive Biotechnologies for immunosequencing. The level of TCR diversity was assessed at day 90 for 22 patients (13 male, 9 female) who underwent HCT. This cohort had a follow-up time for PFS of median=18.5 months (IQR, 10 to 33 months), ranging from 6.0 months to 52 months. Acute GVHD was evident in 59% of the patients and the same percentage exhibited chronic GVHD. Additional samples were available for immunosequencing for 18 patients (10 male, 8 female) from day 180 post HCT. The median PFS for this dataset was 23.5 months (IQR, 10 to 33 months), ranging from 6 to 50 months; 61% of these patients developed acute GVHD and 56% exhibited chronic GVHD.
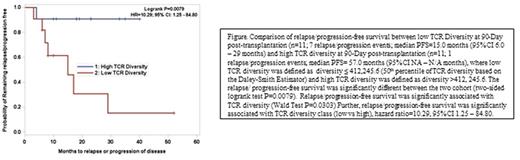
RESULTS: Day 90 post TCR diversity (median=412,245.6; IQR, 81,615.7 to 666,525.8) was significantly associated with relapse/progression of disease when either the 25th percentile cutoff value (TCR diversity ≤ 81,615.7) (hazard ratio=5.60, 95% CI 1.10 - 28.49, and logrank test P=0.0198) or the 50th percentile cutoff value (TCR diversity ≤ 412,245.6) (hazard ratio=10.29, 95% CI 1.25 - 84.80 and logrank test P=0.0079) were reported. In contrast, this approach did not find a significant association between Day 180 post TCR diversity (median=175,453.9; IQR, 94,715.3 to 501,422.4) and risk of subsequent relapse/progression of disease for either the 25th or 50th percentile cutoff values.
CONCLUSION: Measuring the extent of TCR diversity at 90 days post-allogeneic HCT in multiple myeloma patients correlates with the risk of eventual relapse. This potential diagnostic tool could serve as the basis for early interventions to boost the level of donor T cells and to expand the repertoire, perhaps by delayed donor infusions, in order to prevent malignant relapse.
McKiernan: Novartis: Speakers Bureau. Emerson: Adaptive Biotechnologies: Employment, Other: Equity ownership. Vignali: Adaptive Biotechnologies: Employment. Rubinstein: Adaptive Biotechnologies: Employment. Robins: Adaptive Biotechnologies: Employment, Equity Ownership, Membership on an entity's Board of Directors or advisory committees, Patents & Royalties. Siegel: Merck: Consultancy; Celgene, Takeda, Amgen Inc, Novartis and BMS: Consultancy, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal